Most businesses would jump at the opportunity to invest a dollar that saves them $5.85 over the next three years and then keeps on returning savings, all the while improving service to their customers.
That’s what the state of Colorado accomplished by upgrading family planning services between 2009 and 2014, and other jurisdictions have reported even greater returns over the long run. For instance, when Delaware governor Jack Markell saw Colorado’s results, he got excited and kicked off a copycat process of retooling family planning services across his state, where over 60 percent of pregnancies were unintended. Will Oregon and Washington follow suit?
The Colorado success story, by the numbers
Almost half of Colorado women who got pregnant in 2008 said that the pregnancy happened sooner than they wanted or that they hadn’t wanted to get pregnant at all. That was similar to the US average: the rate of unintended pregnancy has been stuck around 50 percent since the 1960s.
Global health experts call unintended pregnancy an epidemic because it’s so common, and the toll on physical health, mental health, and child development so large. A cascade of benefits follow from reducing unsought pregnancies: better health and education for women, more financial security for families, healthier babies, and less strain on social services dedicated to helping families with lower incomes or wealth.
After implementation of the Colorado Family Planning Initiative, teen births and abortions dropped by nearly half.
Public health experts have known this for decades, and evidence showing the protective benefits of intentional parenthood keeps pouring in. The challenge has been how to move the dial. That’s why Colorado’s success caught experts’ attention worldwide.
After implementation of the Colorado Family Planning Initiative, teen births and abortions dropped by nearly half. They fell by nearly 20 percent among women aged 20-24. (Note: Under normal circumstances, over 80 percent of teen pregnancies and 70 percent of pregnancies among single women aged 20-29 are unsought, so this change means women’s realities are better matching their family desires.) Second-order births to teens—teens who gave birth a second or third time—dropped by 58 percent. High-risk births, including preterm births, also diminished.
Poor families benefited the most, because unsought pregnancy is four times as common and unsought birth seven times as common among poor women as among their more prosperous peers. With fewer families facing the dire circumstances triggered by an unexpected pregnancy or unplanned birth, the state saved $66-70 million in public assistance, according to a team of economists at the University of Colorado.

Reduced unintended pregnancy by Good Works Group. (Used with permission.)
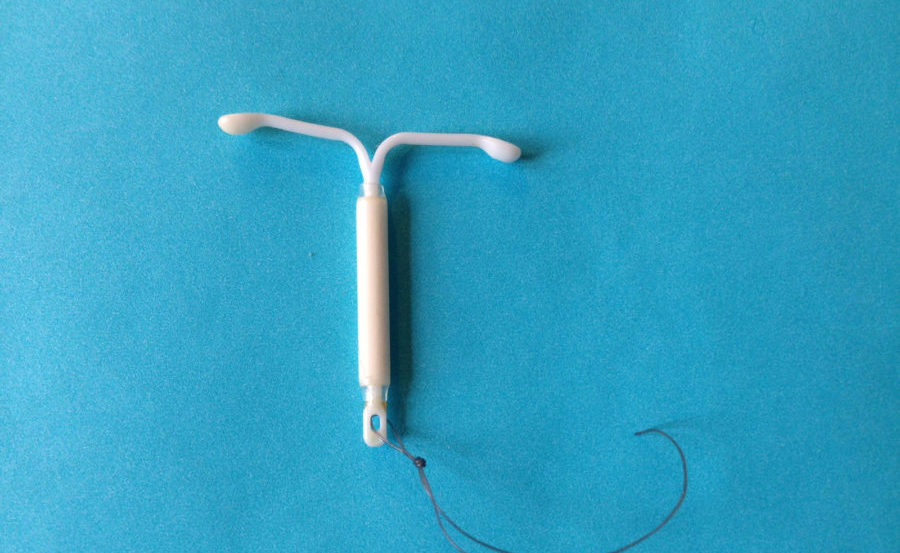
How Colorado did it: LARCs as the lynchpin
How did Colorado get such dramatic results? Much of the improvement came from a technology revolution in contraception. Couples switched away from error-prone family planning methods that require action every day or every time they have sex—methods like pills and condoms (and crossed fingers)—to long-acting IUDs and implants that make pregnancy prevention easy. These methods are “get it and forget it.” They eliminate contraceptive challenges such as ponying up for pills year after year, or just remembering to take it daily, and they work 20-50 times better than the pill. When a woman wants to get pregnant, her healthcare provider can remove the implant or IUD, usually in a five-minute procedure, and normal fertility returns almost immediately.
A study of 9,000 women called the Contraceptive Choice Project and conducted by Washington University in St. Louis demonstrated that long-acting contraceptives dramatically reduce unplanned births and abortions. It also showed that most women prefer these technologies when high cost and other barriers are removed.
In recent years, protective agencies such as the US Centers for Disease Control and Prevention (CDC) and professional groups such as the American Congress of Obstetricians and Gynecologists have declared these methods far more effective and safer than any other method—even for teens and women who are HIV-positive—and far safer than the risks from pregnancy itself. One of these methods, the hormonal IUD, has bonus health benefits, including protection against some cancers.
But for implants and IUDs to become widely available and popular among Colorado women, health agencies had to upgrade their system of care. And that’s what they did.
The Colorado Department of Public Health and Environment, in partnership with an anonymous philanthropic foundation, launched a process of retooling the state’s clinic system to provide state-of-the-art care. Together, they expanded the range of clinicians and facilities that offer contraceptive care, retrained counselors and providers, updated scheduling and billing practices, and launched a public awareness campaign.

Birth Control Effectiveness Chart by Bedsider (Used under a creative commons license.)
Colorado’s four foundational strategies
The Colorado Family Planning Initiative (CFPI) organized around four strategies.
- Increase access to quality services. CFPI adopted a “no wrong door” approach that brought services to women wherever they might encounter the healthcare system. Grants to over 100 public health centers, including school-based and rural clinics, supported training for residents, advanced practice nurses, and others, allowing them to improve counseling and to insert (and remove) implants and IUDs. More flexible hours at these health centers improved access for working women. CFPI integrated family planning into primary care, labor and delivery, and post-abortion care.
- Increase availability of IUDs and Implants. CFPI funding made all methods available with no co-pay, a standard that later would be incorporated into Obamacare (now on the chopping block, of course). Implants and IUDs are cheaper in the long run than other forms of birth control, especially if you include the costs associated with an unplanned pregnancy. But until recently, the up-front price of long acting contraceptives has made these methods unavailable to many women.
- Promote healthy decisions and planning. Better access to better birth control doesn’t do much good if people don’t know about it, so the CFPI worked to normalize conversations about sexual health. Young Latinas, who have a higher-than-average teen pregnancy rate, talked with each other in culturally proficient after-school programs. Social service agencies offered sexuality workshops or provided onsite access to educators. A website, BeforePlay, offered practical information about contraception and sexual health, as well as specific resources available across the state.
- Improve public policy and practices. When it came to building the policy framework for intentional parenthood, advocacy organizations, public agencies, and legislators all played their part. Data from Denver Health and the University of Colorado led the state to change reimbursement policies so that women could get an IUD or implant of their choice immediately postpartum in hospitals. The state Department of Education is developing new standards, and about a third of Colorado children now receive age-appropriate, science-based sexual health education. Despite objections from some religious conservatives, the Colorado State legislature extended funding for the updated health services.
The key to Colorado’s success lies in the interplay between these four strategies. The result has been a dramatic shift toward intentional parenthood as a new norm, one that empowers young people to live lives of their choosing and helps Colorado families to flourish.
A model for the Pacific Northwest to follow
At the start of CFPI, teen and unintended pregnancy in Colorado were significantly worse than in the Pacific Northwest. Now they are nose-to-nose. So, the question is whether Cascadia will deploy some of Colorado’s methods to leap ahead.
Today, despite improvements, Oregon and Washington (and Colorado, too) would still be considered part of the global unintended pregnancy epidemic. In contrast to most of Europe, rates of unsought pregnancy in Washington and Oregon remain close to 50 percent. (Note: More recent state figures put unintended pregnancy in Washington at 37 percent because of a change in the way it is measured. The new figure does not count women who were “unsure” if the pregnancy was intended.)
Groundwork in Oregon
Although Oregon has not yet launched a state-wide initiative akin to Colorado’s, Governor Kate Brown recently affirmed that she and the Oregon Health Authority “place a high priority on improving women’s health and reducing unintended pregnancies by implementing pregnancy intention screenings and providing effective contraceptives to women who do not wish to become pregnant.” Oregon nonprofits, public agencies, and care systems are moving forward on both fronts.
Pregnancy intentions screening: The Oregon Foundation for Reproductive Health has developed a technique—now a national model—that makes it easier for primary care, chronic care, and mental health providers to open up conversations about family planning. It is called One Key Question, and the question is: Would you like to get pregnant in the next year? If a woman says yes, this leads to a conversation about preparing for a healthy pregnancy, called “preconception care.”. If she says no, she has an opportunity to explore contraceptive options, including top-tier methods that might not be familiar. If she says I’m not sure or I’m ok either way, she receives both.
Contraceptive access: In January 2016, two new laws went into effect in Oregon expanding access to oral contraceptives. Following a California model, retail pharmacists can now prescribe oral contraceptives or patches. A second law, the first in the nation, requires insurers to cover a 12-month supply of birth control at a single prescription fill.
Aligning incentives: In 2015, Oregon began to assess how many women served by regional Coordinated Care Organizations receive contraceptives that are considered “more effective” (like pills) or “most effective” (like implants and IUDs). This new measure allows the Oregon Health Authority to link payments to high-quality care.
Setting standards: The summer of 2017 will see the publication of new quality guidelines for family planning care along with self-assessment tools to be used by care systems. The advisory council creating these guidelines includes representation from the state, local, and private and public health sectors. The council has the goal of providing primary care and family planning clinics with clear, state-of-the-art standards of excellence for contraceptive care.
In 2016, the Population Institute, an international nonprofit that promotes high-quality and voluntary family planning services graded Oregon in its top tier for reproductive health and rights, second only to California. The grading system covers effectiveness, prevention, affordability, and access. Several factors contributed to Oregon’s positive rating, including a mandate for comprehensive sexual health education in public schools and expansion of family planning coverage through Medicaid.
But part of the reason Oregon rated well is because the United States as a whole rates so badly. Despite promising trends, the US teen pregnancy rate is far higher than any of the other 34 countries in the Organization for Economic Cooperation and Development. Oregon’s rate is 44 per 1,000—below the national average of 52 but still leaving plenty of room for improvement. Across all age groups, the percent of Oregon pregnancies that are unsought—46 percent—also leaves room for improvement. What would it take to establish a norm of intentional parenthood in Oregon?
Next Steps for Oregon
With national healthcare policy hanging in the balance, Oregon officials may have to scramble to protect residents against funding cuts that could make things worse: a reversal of Medicaid expansion, elimination of the ACA’s contraceptive mandate, cuts to Title 10, or defunding Planned Parenthood. But regardless of how these funding issues play out, there will be opportunities to increase intentional parenthood in Oregon through practice improvements and better public awareness.
Oregon’s One Key Question is a case of “local kid done good,” and by implementing the model statewide, Oregon has the chance to become a national leader in healthcare integration. This will mean incorporating routine pregnancy-intentions screening into primary care, labor and delivery, chronic care, mental health, and drug treatment programs—and doing so in a way that reduces rather than increases the burden on already harried physicians.
To reap the full benefits, clinical settings across the state will need to retool to be fully capable to support IUDs and implants, so that women can obtain the family planning methods they desire with minimal barriers. Upstream USA and the Bixby Center at the University of California San Francisco offer evidence-based training and consultation to help clinic team members streamline scheduling and billing procedures, improve contraceptive counseling, and get skilled at inserting implants and IUDs.
Lastly, the story must be told. Metrics that document downstream cost savings and improved wellbeing will help build durable public support for these programs and ensure that savings can be invested in other services for Oregon families.
Groundwork in Washington
Public officials in Washington have paid close attention to the models in St. Louis, Colorado, and Delaware, and they are keenly aware that better pregnancy prevention and birth timing can improve lives.
Like Oregon Governor Brown, Washington Governor Jay Inslee’s office has voiced support for upgrading contraceptive care statewide. The governor’s Results WA measures aim to reduce unintended pregnancy by 10 percent in five years, recognizing that achieving this goal will likely require broader and easier access to implants and IUDs. When Planned Parenthood showed that low reimbursement for IUD insertions had become an obstacle for clinics serving poor women, the state changed reimbursement rates.
Local and regional players also have stepped forward to upgrade contraceptive services and facilitate a technology shift to “get it and forget it” contraceptives for those who want them:
- School-based clinics in Seattle now offer the full-range of birth control options to high school students, and Neighborcare Health, which runs several of these clinics, employs educators who help teens and their parents explore options.
- The North Sound Accountable Community of Health, which is a front runner in Washington’s Medicaid Transformation process, has launched a series of continuing education trainings to ensure that clinicians in small and rural clinics can provide state-of-the-art care: initiating conversations about pregnancy desires, counseling women effectively about pre-conception health and family planning options, and providing implants and IUDs as desired.
- King County, the state’s most populous county and home of Seattle, has a miracle of its own: a 55 percent drop in teen pregnancy over seven years. Although some factors are unknown, this didn’t happen by chance. In 2008, King County Public Health secured a small grant to train and provide technical assistance to school-based health centers so they could offer IUDs and implants on-site, with follow-up support from Public Health. Three of these health centers hired half-time sexual health educators, who taught in biology and health classes, and provided contraceptive counseling to teens and their parents. These services currently only reach Seattle teens, but the Best Start for Kids levy will help fund new school-based health centers in other King County cities. Not content to stop there, the County Executive’s office and Public Health Department have convened a team of experts—Title X family planning providers, community health centers, school-based health centers, and University of Washington’s Family Planning Division—with the mission to improve birth timing and reduce health disparities for local families.
Next Steps for Washington
Like Oregon, Washington gets high marks from the Population Institute, but statistics on teen and unintended pregnancy remind us that those high marks are rather like being near the top of the class in a B-grade school. The stats on teen pregnancy (47 out of 1,000) and the percent of pregnancies that are unintended (48 percent) come in slightly worse than Washington’s West Coast neighbors.
Routine screening for pregnancy intentions and a statewide upgrade of contraceptive services, if coupled with a public awareness campaign, could radically change those figures. Proven practices from local front runners like Neighborcare’s school-based clinics and the North Sound clinician training project could be inserted into the Medication Transformation process as it rolls out across the state. The Upstream model for retooling clinic practices could become a “shovel-ready” optional project adopted by Accountable Communities of Health across the state.
Changes like these would mesh well with another Washington State imperative—addressing the epidemic of opioid addiction. Neonatal care units are overflowing with newborns suffering from Neonatal Abstinence Syndrome, a form of withdrawal. But much of this suffering could be prevented if more priority were given to helping addicted women manage their fertility. Eighty-six percent of pregnancies in opioid-addicted women are unintended, suggesting that simply helping them to not get pregnant when they don’t want to could prevent a significant part of this suffering.
Looking to the Future
Within a few decades, a surprise pregnancy may actually be surprising. Men likely will have contraceptive options that rival those of women today, and intimacy won’t feel like a roll of the reproductive dice. Nobody will be forced to take action every day or every time they have sex for decades on end simply to prevent ill-conceived pregnancy. With long-acting methods offering years of protection and with each person in charge of his or her own fertility, children will come into the world by the mutual consent of two people who want to create a child together. Intentional parenthood will become the norm. This is the shape of the future.
Today, better birth control for men has yet to emerge from the laboratory, but that doesn’t mean we are stuck. States like Colorado and Delaware are moving rapidly in the direction of intentional parenthood simply by ensuring that all people have access to the information and tools currently available.
In the next few years, Washington and Oregon thought leaders will face policy and health delivery choices that could either stall improvements now underway or accelerate our own trajectory toward intentional parenthood. With Colorado’s model in front of us, the possibilities are exciting.










Comments