When Plan B emergency contraceptives became available without a prescription, I sent my teenage daughter, Marley, and her friend Amanda out to do a little research. Was the medication available in our local pharmacies? What would happen if they asked for help?
Most of the drugstores the girls visited in their meander through Seattle’s Capitol Hill neighborhood kept the medication behind a counter or locked up because it’s so expensive (close to $50 for a single dose). But the pharmacists and retail staff were friendly and eager to help, and the girls came back reporting that the excursion had been fun.
I wish I could say that Marley and Amanda’s experience was typical, but for most teens reality is far different. Capitol Hill is the heart of Seattle’s queer community. It hosts a broad array of immigrants, artists, and homeless young people. The pharmacists there are a flexible, forward-thinking lot—a contrast to some of those in more conservative and rural communities, who have refused to even fill prescriptions for birth control.
On top of that, Marley and Amanda themselves are atypical—girls who have been subjected to years of conversations about reproductive health at the dinner table, thanks to my work in the field. Many teens would have been mortified by the assignment: Ask an adult about birth control? Forget it! Besides, pregnancy is something that happens to other girls, not us.
Skittish Teens + Barriers = Inaction

Most teens feel conflicted about both sexuality and adults (and especially about adult sexuality—but I digress). Curiosity, desire, guilt, anxiety, impulsivity, irritation, dependency—feelings like these create quite a spicy stew in the teenage brain. We all know this, but we don’t always take time to think about the practical implications.
Locked cabinets and prescription requirements require an awkward adolescent to both look some adult in the eyes and cop to sexual activity. They can tip the balance toward denial and inaction, which in turn put girls at risk for unwanted pregnancy.
This means that young women in particular may benefit from a proposal underway to move regular birth control pills from the pharmacy to the drugstore shelf.
No Prescription?
In the United States, the proposal to sell oral contraceptives over the counter has been endorsed by the premier body of relevant experts, the American Congress of Obstetricians and Gynecologists. Ultimately, though, the decision will be made by the FDA.
The FDA came into existence to protect consumer safety and health, but whether a drug is sold over the counter or by prescription can be an artifact of culture and history. In the years after a drug is released, data may accumulate suggesting that it can be safely sold direct to consumers. In fact, most of the top-selling over-the-counter medications, including Aleve, Claritin, Prilosec, Zantac, and Children’s Motrin, once were available only by prescription. But reclassification is complicated. The manufacturer must assemble the research and file a petition with the FDA. The FDA then reviews the evidence related to a set of interrelated questions:
- Can a layperson easily self-diagnose?
- Are instructions easy to follow?
- Is the therapeutic dose easy to monitor without special equipment?
- Is there a low risk of serious side effects, drug interactions, overdose, or abuse?
The goal is to determine whether reclassification benefits outweigh risks, and a growing number of public health advocates say it’s time to make this leap for oral contraceptives. The technology has been around for a half century, and pill formulations have gotten safer and safer during that time. Modern pills that combine estrogen and progestin (called combination oral contraceptives) typically have just a fifth of the estrogen in early pills, and some (called mini-pills) are now entirely estrogen free.
Used Globally, Wanted Here
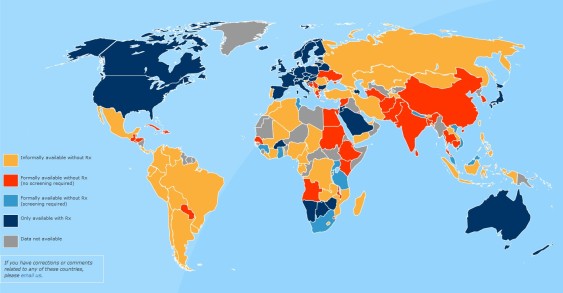
Across the globe, most women can buy birth control pills without a prescription, and the effects seem largely positive. Researchers in El Paso, Texas, studied 500 women who got pills by prescription in the United States and 500 who got pills over the counter across the border. They found that significantly more women who got their pills over the counter stuck with their birth control over the course of nine months.
When asked, US women and teens say they would like this option. A national survey conducted in 2011 reported that one-third of women using a less effective method said they would like to use the pill if it were available over the counter. Notably, interest was highest among young women. In another study, almost half of abortion clients aged 15–17 said they would like to use the pill if it were available over the counter. A key consideration for many young women, even in their 20s, is privacy. Prescription medications require a doctor’s visit, which shows up in Mom and Dad’s mailbox as an insurance statement. With more and more young people dependent on parental insurance through college and beyond, the desire for private options is growing.
Time For A Change
In 2004, a coalition of reproductive health and justice groups, university researchers, and prominent clinicians came together to form the Oral Contraceptives Over-the-Counter Working Group. Their goal was “to reduce disparities in reproductive health care access and outcomes, and to increase opportunities for women to access a safe, effective method of contraception, free of unnecessary control, as part of a healthy sexual and reproductive life.” Ten years later, group leaders believe that regulators and the public may, finally, be ready for the change.
A new California law lets pharmacists provide hormonal contraceptives without a doctor’s prescription. In the Cascadia region, British Columbia often leads the way on social policies that promote health and well-being, but in this case Canada is one of the countries that continues to require prescriptions for hormonal contraceptives, except for emergency contraception. By contrast, Washington is poised for the next wave of change. The state has long been at the forefront in reducing family planning barriers for low-income women, and is one of the few states that does not require a prescription for Medicaid coverage of over-the-counter contraception.
Dr. Daniel Grossman, who coordinates the over-the-counter effort, is optimistic about further change: “Now that a form of emergency contraception is available over the counter for women of all ages, the time is ripe to move the regular birth control pill over the counter as well. The pill is certainly safe enough for over-the-counter use, and it’s likely that improving access to this effective method could help to reduce unintended pregnancy and help women better control their fertility.”
Social Justice
Advocates for young and minority women believe that over-the-counter pills will help the communities they represent.
Deborah Hauser, president of the Washington, D.C.–based Advocates for Youth, has lent the weight of her organization to the working group. Her reasoning is clear: “Young people have the right to lead healthy lives. Transportation, cost, appointment times that conflict with school or work, and the wait to get an appointment all pose barriers for many young women who wish to avoid pregnancy. Improved access to affordable contraception—over the counter and without prior prescription—could go a long way toward reducing many of these barriers and would help young women access birth control when they need it, in the comfort of their local pharmacy or drugstore.”
The National Latina Institute for Reproductive Health also issued a statement in support of the change: “Over-the-counter access will greatly reduce the systemic barriers, like poverty, immigration status and language, that currently prevent Latinas from regularly accessing birth control and result in higher rates of unintended pregnancy.”
Trade-offs

Might reclassifying birth control pills have unintended consequences?
The greatest worry expressed by justice advocates and young women themselves is cost. For example, the $50 price tag on Plan B is a deal breaker for most teens, no matter where or how the medication is sold. Historically, when a medication becomes available over the counter, insurance companies drop coverage. That may be changing, however; in 2000, fewer than a third of HMOs covered any over-the-counter medications; now two-thirds do. In 2013, the US Department of Defense and Bureau of Indian Affairs, in separate actions, decided to cover emergency contraception without a copay or prescription. Each of these changes provides a precedent and a model for ensuring that young and poor women can afford the contraceptives they need.
Interestingly, the greatest worry of reproductive health advocates is that making the pill easier to access may mean young women don’t get information about top-tier long-acting reversible contraceptives, which are 20 times more effective than pills.The very same thing that makes pills a good candidate for over-the-counter sales—the fact that they’ve been around for 50 years—means they’re no longer the top tier of contraceptive technology. Pills have to be taken at the same time every day, which means they’re highly susceptible to human error. In the real world, forgetting, fights, and finances all intrude on the best-laid plans, and consequently women on average miss more than four pills per month. All of this adds up to a one in 11 annual pregnancy rate for women relying on oral contraceptives. Teen girls are even worse than adult women at pill taking; most who start taking the pill are not doing so a year later.
When the Oral Contraceptives Over the Counter Working Group first formed 10 years ago, pills were among the most effective contraceptives available to teen girls. But the new top tier consists of long-acting reversible contraceptives, such as IUDs and implants. In 2012, the American Congress of Obstetricians and Gynecologists recommended these methods as safe and effective for teens.
The difference can be dramatic. When 9,000 St. Louis women were offered the contraceptive of their choice for free, almost 75 percent chose a long-acting reversible contraceptive, and two years later the birth rate for teens in this group was 6 per 1,000—dramatically lower than the national average of 34 per 1,000. Small wonder, then, that medical providers want a chance to tell teens the good news about better birth control.
A “Yes-And” Approach
That said, California may provide the best model. The state is moving forward simultaneously to get the word out about long-acting reversible contraceptives and to make pills accessible and affordable without a doctor’s prescription. The rationale: no one method works for everyone, and women, including teens, do best when they have options.
Thank you to Daniel Grossman of Ibis Reproductive Health for input on this post.


Comments are closed.